Grafting Lower First Molars
Two Different Strategies and Techniques
Abstract
Lower first molars are far and away one of the most common teeth in general for a patient to be missing. In addition, a missing lower first molar is also the tooth most likely to cause dramatic shifting of adjacent and opposing teeth. It has been stated that lower first molars provide a large percentage of the posterior occlusal surfaces needed for proper mastication (Ref 1). When this tooth is missing, chewing becomes significantly more inefficient and this leads to adjacent teeth carrying larger occlusal loads. Missing lower first molars can have dramatic effects occlusally and can create situations that can cause further harm to the entire dentition (Ref 2).
There are 2 basic reasons that lower first molars are likely to need extraction or be missing. First, because these teeth are the first posterior permanent teeth to erupt, they are more likely to acquire decay earlier in life. Secondly, these teeth must absorb a massive amount of continual occlusal stress throughout life, which often leads to future fractures, root canals, and crowns. Due to these continual insults, lower first molars are likely to require restorations earlier in life as well as more extensive restorations later. Because of this restorative “death spiral”, it is not uncommon for a lower first molar to be missing and subsequently, an implant to be placed.
Implants have become the gold standard for replacing these teeth and successful bone grafting techniques are a crucial step in ensuring a suitable site for future implant placement (Ref 3,4,5). Simple grafting techniques are invaluable to all dentists who extract teeth and want to preserve acceptable bony architecture for future implant placements. This article illustrates 2 separate socket grafting scenarios and solutions that dentists can use for creating future implant sites with acceptable bone quality and quantity.
Keywords: Extraction, site preservation, atraumatic, grafting, barrier membrane
Case 1: Socket preservation with non-resorbable PTFE membrane
The patient presented for an emergency exam with pain and swelling that seemed to be emanating from tooth #30. A “J” shaped apical lesion and a buccal furcation probing depth of 12+ mm confirmed a fatal root fracture and the need for extraction. (Figs. 1,2,3).



Fig. 3 – Lingual gingival recession and inflammation.

Fig. 4 – Tooth #30 post extraction illustrating and con- firming complete removal of all root structures
Before the tooth was extracted, the patient expressed the desire to have the tooth replaced in the future with an implant. It was discussed that the socket would need to be grafted immediately after extraction in order to preserve bone and have a site acceptable for a successful implant in the future. The patient was anesthetized with lidocaine and bupivicaine. The tooth was removed easily in 2 pieces (Fig. 4) and the socket debrided completely of all residual granulation tissue. It is noted that aggressive debridement of residual granulation tissues is absolutely imperative for successful socket grafting. If any cystic tissue is left within the socket, this can lead to areas of insufficient bone growth, deficient quality and cause future complications.
After successful degranulation, the socket walls were evaluated using a periodontal probe to determine the extent of bone destruction. The buccal wall was found to be damaged to the point that there was a bony defect that extended apically approximately 10 mm (Fig. 5). Because this type defect has difficulty preventing epithelial ingrowth into the graft, a resorbable membrane was required to insulate the graft material from the buccal gingiva during the future healing period. By using a surgical curette and a tunnel approach on both the buccal and lingual aspects, an envelope flap was created to allow space for the placement of the membrane.
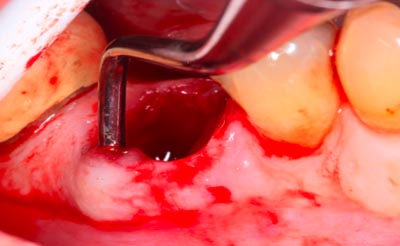
Fig 5 – Post extraction socket # 30. Probe illustrating significant buc- cal wall defect requiring a membrane barrier for successful grafting.

Fig 6 – PTFE resorbable membrane (Cytoplast TXT-200, Osteogenics Biomedical)

Fig 7 – PTFE resorbable membrane customized and cut to match the shape of the extraction socket.
Because the buccal plate was absent due to long standing infection and periodical pathology, the need for a barrier membrane was imperative for the long term success of the bone graft. It is important for the reader to remember that soft tissue heals much faster than hard tissue and this type barrier would exclude the invagination of epithelial cells into the newly placed graft. A cytoplast PTFE non-resorbable membrane (Osteogenics Biomedical TXT-200 Singles) was chosen for this site specifically for its durability and ability to withstand exposure (Fig. 6). The graft area was measured and the membrane trimmed to ensure complete coverage of the graft area (Fig. 7). Because the width of the socket was 9mm, the membrane was trimmed to 10 mm at its narrowest portion so as to cover the socket completely and tuck the ends under the medial and distal papillae (Fig 8).
The membrane was first tucked deep into the buccal aspect of the envelope flap with care taken not to allow the membrane to fold over on itself. Tucking one corner first sometimes makes membrane insertion easier. It is critical that the membrane be placed so that all soft tissues are isolated from the graft to ensure that there will be no epithelial migration into the graft itself. Once the membrane was secured into the buccal flap, a cortical-cancellous mix bone graft material (Creos- Nobel Biocare) was placed in the socket (Fig. 9). After the socket was completely filled, the membrane was flipped over and tucked into the lingual aspect of the envelope flap so the entire graft was completely isolated from any soft tissues. The flaps were closed using a Vicryl suture. Multiple loops creating a mesh type netting across the coronal portion of the socket ensured complete enclosure and stability of the membrane for 6 weeks healing time (Fig. 10). After 6 weeks, the membrane was removed non surgically with pliers and the graft left to heal completely for 12 more weeks before the implant was placed.

Fig 8
After reflection of buccal ginvia apically and towards adjacent teeth, PTFE resorbable membrane inserted into the flap area. It is important to note that all aspects of the buccal bony defect were covered by the membrane barrier, preventing epithelial migration into the graft area.
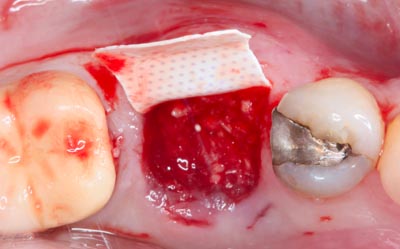
Fig 9
Particulate corti- cal-cancellous bone graft (Creos-Nobel biocare) placed within the extraction socket and completely pro- tected on the buccal from possible gingival migration.
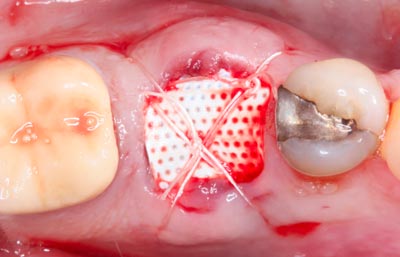
Fig 10
Final position of PTFE membrane secured in place with Vicryl monofilament cross suture closure.
“ Simple grafting techniques are invaluable to all dentists ”
Case 2: Socket preservation with collagen/cyanoacrylate plug
The patient presented with tooth #30 infected with furcation involvement. The PA suggested that any attempt to save the tooth would be precarious at best (Figs. 11,12).The tooth was deemed non-restorable and a treatment plan for extraction and immediate grafting was accepted by the patient. The patient was anesthetized with 1 carpule lidocaine and 2 carpules bupivicaine to ensure that any post-operative pain would be minimized.
The tooth was sectioned completely through the furcation in an attempt to extract the tooth with minimal damage to the bony socket (Fig.13). Even though the tooth roots fractured and came out in pieces, the socket was left intact and all bony walls were not disturbed (Figs.14,15,16). Because the socket was left completely intact, including the buccal plate, a simple grafting/socket preservation technique could be implemented and the use of a membrane barrier avoided. The socket was completely derided of any residual granulation tissue and irrigated thoroughly with sterile saline.
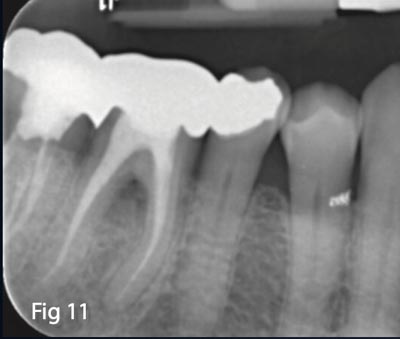




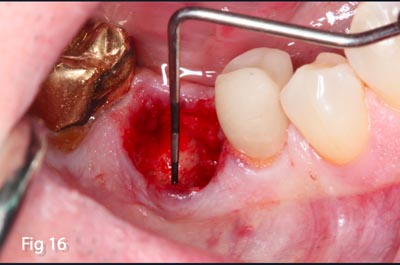
Fig. 11,12 – Pre op PA tooth #30 illustrating furcation involvement and fatal root fracture.
Fig. 13 – Tooth #30 sectioned B-L to facilitate extraction.
Figs. 14,15 – All roots and tooth fragments removed and granulation tissue observed within the socket.
Fig. 16 – Probing confirms the preservation of the buccal bony plate and complete degranulation of socket. This ex-
amination and evaluation confirms the correct choice of a simple socket preservation technique as opposed to the
need of a barrier membrane to prevent epithelium migration into the graft site.
A makeshift membrane was made using a collagen plug coated in cyanoacrylate liquid (PeriAcryl- Glustitch). The collagen plug was first compressed into a disc the approximate diameter of the socket and then coated with the PeriAcryl adhesive (Figs. 17,18,19).

Fig. 17 – CollaPlug, Absorbable collagen dressing (Salvin).
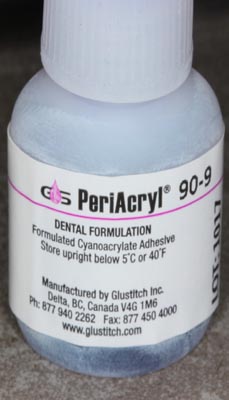
Fig. 18 – PeriAcryl cyanoacrylate adhesive (Glustitch Inc.).

Fig. 19 – CollaPlug compressed and modified with PeriAcryl.
This barrier was allowed to dry for 10 minutes. The socket was filled completely with cortical/cancellous bone graft (Creos- Nobel Biocare) and the graft covered with the now hardened collagen plug barrier and suture in place with a looping chromic gut suture (Figs. 20,21). The plug was left in place for a period of 2 weeks before it ejected on its own, leaving the graft in place for a healing period of 12 weeks before implant placement(Figs. 22,23).

Fig. 20 – Post extraction site grafted completely with particulate allograft (Creos- Nobel Biocare)

Fig. 22 – Grafted site #30, 2 weeks post-op illustrat- ing complete socket preservation and excellent site preservation for future implant placement.

Fig. 21 – Grafted socket covered with Peri-Acryl mod- ified CollaPlug collagen covering, secured in place with chromic gut crossed sutures.

Fig. 23 – Grafted site #30, 2 weeks post-op. Note adequate socket closure and complete retention of graft material leading to satisfactory B-L ridge width for future implant placement.
Conclusion
All dentists need to be well versed in grafting procedures that prevent bony atrophy and lead to acceptable implant sites. The simplification of these grafting techniques give dentists the skills and knowledge to confidently preserve immediate traction sites competently, confidently, and consistently.